My Story
I’m Brendan Lovel from Perth WA. I’m a bloke with a message for every man from aged 50.
This is my story of how I procrastinated and should have acted faster on my increasing PSA Readings, finally having an Ultrasound, an MRI and a Biopsy that revealed a 60% mildly to moderately aggressive cancer, which had to be removed in less than 3 months or it could have spread outside.
Helpful Facts
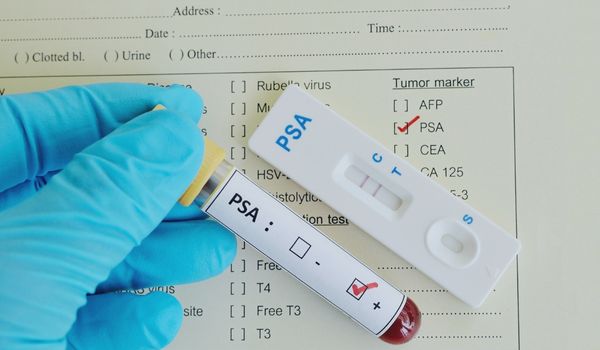
- PSA (Prostate Specific Antigen) – an enzyme in the blood.
- Elevated levels of PSA can help identify issues like cancer and infection.
- It is a simple blood test you can have with your yearly check-up and covered by Medicare. (12 monthly).
- Enlargement isn’t always a sign of cancer. The prostate enlarges as men age.
- Most prostate cancer usually progresses very slowly. It can take up to 15 years to spread out of the prostate. However, it can also be mild to moderate to highly aggressive and can grow and spread quickly out from the prostate. Prostate cancer is usually asymptomatic(no signs)
- An MRI combined with a blood test and a Digital rectal exam is the best front-line test to detect or rule out prostate cancer.
- The risk increases from 50 onwards. 40 onwards if you have a family history.
- 66 is the average age for Prostate Cancer diagnosis.
- 1 in 11 men will develop it by age 70.
- 1 in 7 men is diagnosed with it by 75.
- 1 in 6 men is diagnosed with it by 85.
A Full Account of My Journey
My Starting PSA Numbers
13/11/2013 MY PSA READING WAS 1.91.
25/08/2016 MY PSA READING WAS 2.01.
My Prostate was not checked in 2017/18 but then I had not asked for it to be checked. You must ask your doctor for a PSA test.
I have blood tests every year at check-up time in August so it would not have been an issue to add my PSA every year given I was in my sixties.
This went unnoticed due to other stuff getting in the way!
How could any ‘other stuff’ be more important than my health?
2018 I was 65. My GP with a couple of months’ notice relocated to another clinic. He did me a favour in hindsight. I was seeing him about cholesterol levels, shingles, anxiety and sleeping issues and a Health Plan but my highest health risk was and proved to be Prostate cancer.
14/9/2019 MY PSA READING WAS 2.95.
Symptoms
My Symptoms – I couldn’t empty fully when peeing. I had to repeat. Pee – Repeat Pee! I was getting up to pee during the night. Sometimes I could not pee and would have to try a bit later. Nothing new for many men!
My new very diligent GP found my prostate was enlarged by finger examination (Yes – do not avoid doing this – it doesn’t hurt – just feels uncomfortable!) and said I might consider medication and/or a rebore to help me pee better!
Crikey a rebore sounded painful! You may be familiar with this already.
But my PSA was low I thought, and I was not that concerned about my peeing problem. My Prostate was increasing in size, but not becoming an increasing problem. I had just been peeing, repeat more pee repeat for at least 2 years and I’d become used to it. I had other more important issues to worry about!
I had put off any action early in 2020 due to my son’s wedding and a serious family Matter...... then Covid hit – it was easy to put it off then.
9/6/2020 MY PSA READING WAS 3.30.
Luckily my new very diligent GP said I needed an ultrasound in Sept 2020 which quantified my peeing issue.
My GP encouraged me at my follow up appointment to go to a Urologist. You would think that I would have sought a referral to a Urologist then but no I let other stuff get in the way again!
Increasing PSA Numbers and Taking Action
28/10/20 MY PSA READING WAS 3.74.
Alarm bells should have been ringing at this point due to the percentage increase. My pathology report stated: ‘Current PSA is within normal limits’. ‘However, a normal PSA does not preclude cancer’.
My last two readings were over 3 so thanks to a Medicare change in 2018 a Urologist can now refer you for an MRI at this stage for clarification on the status of your prostate. An MRI will determine cancer or no cancer but not the type of cancer.
Feb 21, 2021 Finally an appointment with my GP suggested Urologist!
End of March 2021 I Had an MRI to ascertain what the status of my Prostate was.
More delays at this time due to a lack of communication with my first Urologist’s office about arranging an appointment with me to discuss my MRI results when they arrived. A message was missed while away for a few days. More time had elapsed.
Late April 2021 – Finally I had an appointment with my Urologist who confirmed from the MRI - a LESION (tumour) on my Prostate.
This first Urologist who my GP had referred me to had spoken of having a biopsy to further determine the nature of the lesion.
Fortunately, my wife had found out about an especially highly regarded urologist who had brought Robotic Prostate surgery to St John’s Hospital Subiaco WA so I moved to him for a second analysis of my MRI results.
My second opinion Urologist also suggested moving ASAP to a biopsy.
My wife (a nurse) and I were highly impressed by this Urologist and his office’s efficiency. He could show on two screens my MRI in detail.
IMPORTANT LESSON
Don’t put up with much delay for appointments if like me your PSA is seriously rising – even if it seems low.
Don’t put off making an appointment - it’s your life and time may be of the essence!
If you have a cancer on your prostate it won’t wait!
Biopsy and the Diagnosis
END OF MAY 2021 – BIOPSY.
My Biopsy at end of May showed a (mildly to moderate) aggressive cancer (Gleason score 4 plus 3) and my Urologist said it should be taken out or have radiation within 3 months! 60% of my cancer was mildly to moderately aggressive so it was quite urgent. He told me it may have only been growing for a couple of years.
We had to act within the 3 months to avoid the cancer spreading outside my prostate.
Shock set in for my wife and I. Decision making immediately became harder, but decisions had to be made urgently.
My low PSA and seeming slow increases had fooled me and I was now one of the 1 in 7 guys who had to take action on a mildly to moderate aggressive cancer.
Apparently, it was still contained in my Prostate gland which was the good news.
The odds seemed good but well I was now one of those 1 in 7 guys who are diagnosed with Prostate Cancer. I felt rather unlucky especially already having had CLL (Chronic Lymphocyte Leukaemia.) diagnosed at 43.
So we took a few days to consider the options being removal or radiation!
Decision Time
Due to my Chronic Lymphocyte Leukaemia, I really had no choice. Removal it had to be.
Crikey, I was in a state trying to get my head around this diagnosis.
How could this be my lot?
I felt sorry for myself and for my wife. Why me? How would I explain this to my 6 children? I let them know carefully so as not to overly concern them.
I didn’t recognise it easily, but I was very, very angry inside.
My anxiety level went through the roof off an already quite high base. A few days after diagnosis, I went to my GP and he prescribed a mild anti-depressant to settle me down. This was the first anti-depressant I’d ever taken.
Emotions
I’m not sure, but a combination of my diagnosis plus possibly a known side effect of my anti-depressant began causing reduced libido and orgasm became nearly impossible. Crikey it was affecting my love life already! This created added stress and a sense of what problems there may be the on the other side.
I increasingly had low patience levels at home and especially driving out on the road.
I felt very reactive when other drivers wouldn’t give way at a roundabout, or cut me off, or turned in front of me, or didn’t indicate, or when Google took me a quicker back street/ multi roundabout way, or someone beat me to a carpark!
I felt prickly, cranky, intolerant, and overly sensitive. I had zero patience. This zero patience was despite being on an anti-depressant which had improved my anxiety level substantially!
I felt deeply sad that my gorgeous amazing loving partner of 25 years was now being affected. She is 10 years younger and here I am with a diagnosis that after the surgery affects continence and erectile function and is the total opposite of romance!
Luckily, she is very understanding, and we have a deep love and care for each other.
After trying to act sensibly over timing and another appointment with my Urologist a date was confirmed for him to do a Radical Robotic Prostatectomy on August 27, 7.30am.
Our emotions were so up/down during each day since the diagnosis. We needed a few weeks to process how life might change.
Choosing To ACT
I read everything I could on the subject, had an appointment with Jo Milios a highly renowned Men’s Health Physiotherapist in Perth who specialises in Incontinence in men due to Prostate removal. Once I had seen Jo I remember feeling it was now time to make a decision on the surgery date and we did. I see Jo in a few days to follow up post-surgery on the status of my incontinence which seems significant!
I contacted Cancer Council WA, spoke to a very helpful lady, made an appointment with the Midland branch near me for Reiki and Counselling sessions x 4 both sides of our holiday. The Reiki sessions relaxed me and the counselling was powerful.
Both practitioners were very compassionate and understanding.
We decided to still take our planned trip up North for 3 weeks to see our new grandchild and two of my children and their families.
Time away on holidays was an excellent diversion from the oncoming reality of my operation on August 27 and relaxed us both.
After our holiday I had an appointment with Nurse Practitioner/Sexologist Melissa Hadley Barrett – highly regarded and experienced in helping restore sexual function after Prostate surgery! Melissa was very positive and incredibly sensitive and understanding. This gave me some confidence for the future even before my surgery.
7 days before surgery I had a routine blood test. I bought bowel prep.
The countdown continued – we went down to Margaret River for a beautiful 3 day break the weekend before. The clock was ticking!
A sense of relief developed in the last few days as each day brought it closer - it was time to have the cancer out albeit my prostate gland would have to go with it!
Two days before surgery I was enjoying meals, snacks and a last beer for a while – all tasted fantastic!
The Operation and Being Vulnerable
August 27. 6.15 AM. My wife and I arrive at St John’s Subiaco for admission.
At this point I should say any man in this position would be advised to take a friend or family member if no partner as the prospect is daunting.
By 7.15am I was back in the same spot close to the operating theatre where weeks previously the nurse ironically had asked me before my biopsy, if I was having my prostate out! I said definitely not!
I had a funny cross ward chat with an older man who had just been wheeled in opposite me. He said he was about to have further heart surgery. He seemed quite relaxed. He looked at me and said ‘Happy Days’!
He had a dry sense of humour and we wished each other well for our imminent operations. This interchange was very special and relaxed me.
The anaesthetist came next, and I explained to him that I can get highly claustrophobic when the mask goes on, so he said he would hover it above my face only until I was out! Very reassuring.
I was wheeled into the theatre and apart from the nurse and anaesthetist I spotted Da Vinci the very impressive, large gangly looking robot in white with black trim and its control panel/screen in readiness for my operation under my Surgeons guidance!
My Surgeon came in and spoke very calmly and reassuringly.
I next remember waking up back in my room to see my wife sitting waiting for me.
Strange feeling. My prostate had gone! I soon realised I had a catheter in place!
Next morning my surgeon came in looking all relaxed and casual, he had a look over me, said the operation had gone well but said the catheter straps had slipped down my leg and were a bit of a mess. I laughed as I had not been game to see under the sheet to have a look at this contraption until then.
Later in the morning my wife came for the day. I was feeling very vulnerable and fragile and sad at having had the operation and cried for the first time. I felt deeply emotional, with grief over losing my prostate albeit so necessary, but very lucky to have my wife alongside me.
First Post-Op Days
Two days later I headed home tired and wondering how I’m going to deal with a catheter in for 10 days!
I sat down to meditate the second night home and the gravity of what had happened hit me again – I got teary with the deep emotion I was feeling. I was surprised but not.
Next few days, poor sleeping, afternoon resting, lots of medication, feeling fragile but have enjoyed family for Father’s Day and mates over and realising I’m lucky as so much support from my wife. I don’t underestimate the toll on her as she has lost a lot of sleep, been highly attentive to my needs and seen me struggle through these first days at home.
I’ve been walking around our streets which are flat but missing out on our uphill and down dale much longer aerobic walks with our dog.
The Other Post-op Days: Incontinence
My catheter was removed 10 days after my surgery at the hospital. Then we met the Surgeon for our follow up appointment. He explained it had gone well but my hernia mesh x 2 had made it more challenging. He spoke of the pathology test showing that my cancer was in fact 80% not 60% mildly to moderately aggressive as the Biopsy had indicated showing just how important it had been and lucky that I had the surgery within the 3 months.
On the drive home I felt tired, pad wet already, an odd feeling to be free of the catheter but very relieved to have it out.
The last 7 days I have been ripping through Incontinence pads like tissues during a head cold! My bladder is playing games with me it seems, as some days i do better than others. I need a rest each lunchtime/early afternoon, usually have a sleep for an hour, lay on the bed then get up trying hard to hold on until the toilet.
I get sore doing so many pelvic floor lifts!
In a few days I see Jo Milios my Physio to really determine how I am going.
Also, in a few days I see Melissa Hadley Barrett to begin the work on restoring my sexual function. It’s hard to even imagine at the moment!
From 'Challenging' to 'Opportunity'
A couple of days after my diagnosis I had thought about my diagnosis and said to myself ‘how challenging’ and there and then I decided to use ‘opportunity’ as my word whenever I was about to use/ think the word challenging. So challenging became an opportunity quite often in the weeks since. An opportunity to see my situation in a new light, to find my way through and past incontinence and disrupted sexual function intuitively and with even greater connection with my amazing partner.
My opportunity is also now in My Prostate Cancer story to make a real difference to the lives of many men. I want men to act on my story. Let me know if my story brings up anything for you or makes you act. Don’t put it off!
I feel quite positive much of the time, but it does seem I’m making slow progress currently! After all this I’m still one of the lucky men.
Feel the love and comfort of your family and friends and the care and concern for you by Cancer therapists, counsellors, and the medical professionals.

My MESSAGE to Men
My message men is to have yearly PSA tests. Don’t let FOFO (fear of finding out) stop you or put it off because that happens to other blokes.
If your PSA readings are in the 3’s twice, get a referral to a Urologist fast for an MRI.
Don’t let anything (even other health issues) stop you being tested 12 monthly when over 50 or over 40/45 if you have a family history of Prostate cancer.
Change Urologist if you have any doubts.
Reach out to your mates, even ones you haven’t spoken to for a while or ages and anyone you know who has been through this as they are all gold!
Sources:
- Prostate Cancer Foundation Australia. enquiries@pcfa.org.au
- Cancer Council Australia
- Prostate Cancer Free. prostatecancerfree.org
Having issues with your sex drive, experiencing sexual performance anxiety, erectile dysfunction or another problem down there? Book a consultation with one of our practitioners.
Email admin@rshealth.com.au or click on the button below.